-Acute Respiratory Distress Syndrome-
-Acute Respiratory Distress Syndrome (ARDS) is a distinct type of hypoxemic respiratory failure
-When healthy lungs are disrupted by lung injury, infection, of fluid, there is a disruption of surfactant causing excess fluid in both the interstitial spaces and the alveoli
-The alveolar injury produces alveolar damage and causes release of inflammatory cytokines such as TNF and interleukins
-Damage of the capillary endothelium allows protein to escape from the vascular space. The fluid then pours into the interstitial spaces and overwhelms the lymphatics
-As a result of this there is impairment of gas exchange, decreased lung compliance, and increase pulmonary artery pressure
-Possible etiologies of ARDS include: sepsis, aspiration, pneumonia, trauma, burns, multiple blood transfusions, pancreatitis, drug overdose, near drowning, pulmonary contusion, smoke inhalation, CABG, pulmonary contusion, venous air embolism, drug reaction, amniotic fluid embolism, pulmonary edema, and BOOP
-Signs and symptoms of ARDS typically appear within 6-72 hours of the initial insult or injury and decline rapidly
-Patients typically present dyspnea, cyanosis, hypoxemia, diffuse crackles, tachycardia, diaphoresis, and accessory muscle use. Patients are typically coughing and will have chest pain
-Patients typically are hypoxemic and a wide A-a gradient
-High FiO2 is needed to get desired oxygenation
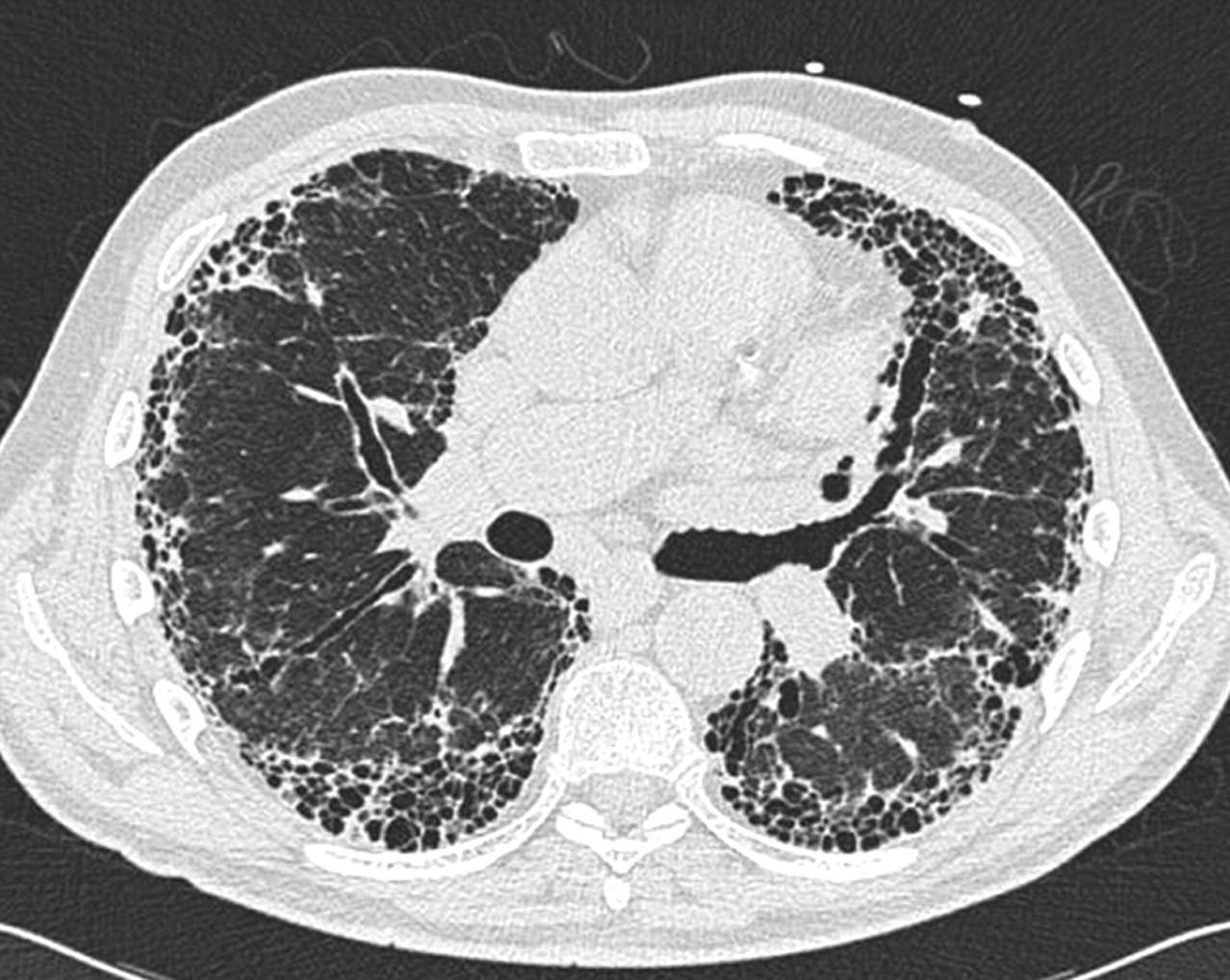
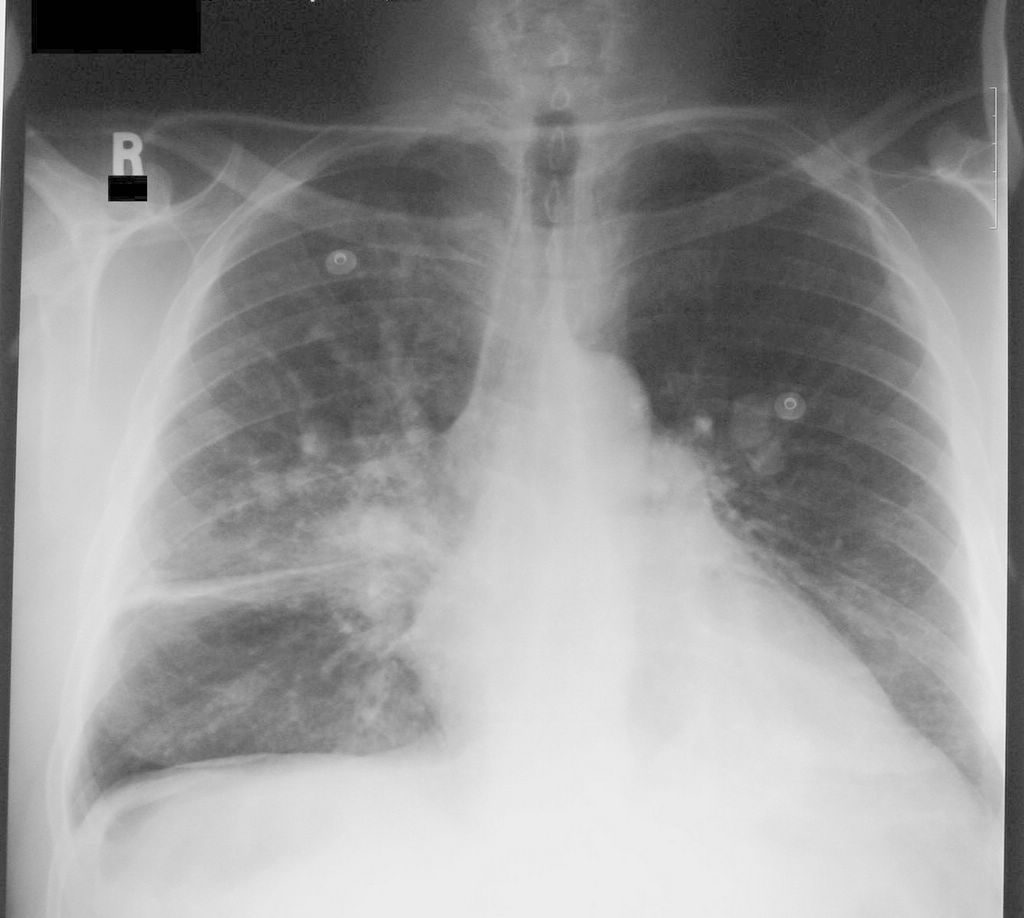
-Chest X Ray typically shows bilateral alveolar infiltrates, and CT scan will show widespread patchy airspace opacities that are more apparent in dependent lung zones. This will likely progress to a ground glass appearance
-Most patients require moderate to high concentration of inspired oxygen over the first several days. The patients who survive will have better oxygenation and decrease in alveolar infiltrates which will allow ventilator weaning to begin
-Complications of ARDS are related to mechanical ventilation: barotrauma, nosocomial pneumonia. May also have delirium, GI bleed due to stress, thrombosis, and catheter related infections
-Once the initial injury or insult is past or treated, the patients who respond can be weaned from the ventilator and FiO2 can be weaned
-Hyaline Membrane Disease-
-Hyaline membrane disease (HMD) is also known as Respiratory Distress Syndrome (RDS) or Infant Respiratory Distress Syndrome (IRDS)
-The pathophysiology behind HMD is that there is a deficiency of surfactant, usually due to prematurity, that reduces the alveolar surface tension, which decreases the pressure needed to keep the alveoli open, and maintain alveolar stability
-When the surfactant is deficient, the infant cannot generated the increased inspiratory pressure to keep the alveoli open, and results in alveolar collapse and diffuse atelectasis
-This subsequently leads to decreased lung capacity and low functional residual capacity. Hypoxemia then results. This may lead to right to left shunting and cause a further VQ mismatch
-Prior to exogenous surfactant administration, uncomplicated HMD typically progressed for 48-72 hours until there was production of endogenous surfactant
-Now with treatment with exogenous surfactant (Survanta), there is dramatic improvement of pulmonary function, and shortening of clinical course. Use of CPAP has improved the clinical course of HMD
-Foreign Body Aspiration-
-Foreign body aspiration is can be potentially a life threatening event
-Foreign bodies are most likely to be aspirated into the right side secondary to the angle of the right mainstem bronchus
-Inorganic material such as glass or metal may cause little tissue inflammation but can result in direct airway injury if they are sharp
-Organic material such as nuts can cause significant inflammation and granulation tissue formation resulting in stenosis
-Aspiration of medications such as iron tablets in pill form can cause airway inflammation and ulceration
-X-Ray may confirm the presence of foreign body; however, direct visualization with bronchoscopy is need for definitive diagnosis and removal.
-In cases of life threatening aspiration initial support should focus on treating the airway and removing the obstruction. If it is above the larynx may be able to be removed with forceps, if below the larynx will need bronchoscopy for removal.