Infectious Disorders-
-
Acute Bronchitis-
-Acute Bronchitis is generally viewed as a self limiting condition, due to upper airway infection
-Patients usually present with a productive cough lasting more than 5 days but less than 3 weeks
-Chronic bronchitis is a productive cough for most the days for at least 3 months in each of two successive years
-Acute Bronchitis is generally caused by a virus
-Usual causes of acute bronchitis are influenza A and B, parainfluenza, coronavirus, rhinovirus, RSV, and human metapneumovirus.
-It has been suggested that bacterial pathogens that cause pneumonia (Strep Pneumoniae, Haemophilus Influenza, Staph Aureus, Moraxella Catarrhalis) can cause bronchitis, but there have been no studies to prove this
-Other organisms that rarely cause acute bronchitis include: mycoplasma pneumoniae, Bordetella Pertussis, Chlamydophilia Pneumoniae
-Symptoms are productive cough, wheezing and may have an associated fever.
-Treatment is directed a symptom control. Albuterol for wheezing and prednisone as needed for an adjunct.
-Indications for chest x ray include a HR greater than 100, RR greater than 24, temperature greater than 38 degrees C, or oxygen saturation less than 94% on room air on healthy adults
-
Acute Bronchiolitis-
-Acute Bronchiolitis is defined as a syndrome that occurs in children less than 2 years of age and presents as rhinorrhea followed by lower respiratory infection with inflammation that results in wheezes and/or crackles
-Acute Bronchiolitis typical is caused by viral pathogens but on occasion can be caused by Mycoplasma Pneumoniae
-Risk factors for developing severe disease with bronchiolitis include: prematurity, age less than 12 weeks, chronic pulmonary disease, congenital and anatomic defects of the airways, congenital heart disease, immunodeficiency, and neurologic disease
-Indications for Hospitalization of Acute Bronchiolitis patients:
1. Signs of respiratory distress nasal flaring, retractions, grunting, RR>70, dyspnea or cyanosis
2. Toxic appearance, poor feeding, lethargy
3. Apnea
4. Hypoxemia
5. Parents who are unable to care for the child at home
-Management includes management of hydration and oxygenation. Bronchodilator therapy and glucocorticoids are indicated if wheezing. Nasal suctioning is also helpful
-As a rule of thumb, antibiotics generally are not indicated in the treatment of acute bronchiolitis
-
Acute Epiglottitis-
-Epiglottis is inflammation of the epiglottis and adjacent supraglottic structures
-Infectious epiglottitis is cellulitis of the epiglottis and its adjacent structures. It can result from direct invasion or from bacteremia
-Once the infection begins, swelling rapidly progresses to involve the entire supraglottic larynx and swelling is halted by the tightly bound epithelium at the level of the vocal cords
-Airway obstruction can result in cardiopulmonary arrest
-Epiglottis can be caused by bacteria, viral, or fungal etiologies
-The most common pathogen of epiglottis is Haemophilus Influenza Type B (HIB)
-We have seen a dramatic decreased in the frequency of epiglottis because of the HIB vaccine
-In immunocompromised patients candidia or pseudomonas can cause epiglottitis
-Other non infectious etiologies include: thermal injury, foreign body ingestion, and caustic ingestion
-Clinical symptoms include: respiratory distress, signs of upper airway obstruction, stridor, sitting in the tripod or sniffing position, and drooling.
-Fever, severe sore throat, odynophagia, and drooling are common
-Chest x ray or soft tissue neck may reveal a "thumb print" sign
-Labs should be deferred until the airway is secured. Labs should include CBC and Blood Culture
-Two main parts of management of epiglottis include securing the airway and instituting antibiotics. Recommended empiric treatment includes third generation cephalosporins with clindamycin or vancomycin.
-
Croup-
-Croup is also known as laryngotracheobronchitis (LTB)
-Croup presents clinically with inspiratory stridor, bark cough, and a hoarse voice.
-Most common ages afflicted are between the ages of 6 months and 3 years of age
-Most common offending organism is the parainfluenza virus
-Typically presents acutely rather than slow onset
-The mainstays of treatment of croup are glucocorticoids and racemic epinephrine
-The Wrestly Croup Score determines treatment and it is based on physical exam
-Severe croup can progress to respiratory failure where there is fatigue, listlessness, marked retractions, decreased breath sounds, decreased LOC, cyanosis, pallor, and tachycardia disproportionate to fever. Rarely this patients may need mechanical ventilation. Capillary blood gas should be obtained
-Mild Croup can be treated at home. Cool mist can provide symptomatic relief
-Children have a tendency to get worse at night. If the child looks bad or may need admission, consider admission especially if in night or evening hours
-Indications for admission of Croup patients include: need for racemic epinephrine continuously, need for oxygen, moderate retractions, degree of response to initial therapy, if they look toxic, poor oral intake, if less than 6 months, return visit in 24 hours, poor parenteral care at home
-Usually resolves itself within 3-7 days
-
Influenza-
-Influenza is an acute respiratory illness caused by the Influenza A and B viruses
-Transmission of the virus is by respiratory secretions
-Generally speaking, viral shedding can be detected 24-48 hours before the onset of symptoms, but much lower during the symptomatic period of the illness
-Uncomplicated influenza presents with fever, headache, myalgias, nasal congestion, non productive cough, and sore throat. Physical exam is usually unremarkable
-Pneumonia is the most common complication of influenza
-Myositis and rhabdomyolysis are also complications of influenza
-CNS complications of influenza include: encephalopathy, encephalitis, transverse myelitis, aseptic meningitis, and Guillain Bare Syndrome
-Two classes of antiviral drugs available for treatment of influenza-
1. Neuraminidase inhibitors such as zanamivir and oseltamivir are active against influenza A and B
2. The adamantanes such as amantadine and rimantadine that are active against influenza A
-These agents can shorten the duration of the illness 12 hours to 3 days. Most studies have shown benefit when instituted 24-48 hours from the onset of symptoms
-Institution of any antivirals is recommended when: illness requiring hospitalization, age over 65, pregnant women or post partum less than 2 weeks, or progressive, severe or complicated illnesses
-High priority age groups for influenza vaccine: pregnancy, immunocompromised patients, healthcare workers and household contacts
-
Pertussis-
-Pertussis is known as the whooping cough
-The organism that causes pertussis is Bordetella Pertussis
-Usually affect children less than 10 years and presents with a prolonged cough, inspiratory whoop, paroxysmal cough, and post-tussive emesis
-Since the pertussis vaccine, more than half of the cases occur in adolescents and adults
-Incubation stage is following exposure is typically 7-10 days but may be 3 weeks or longer
-3 Phases in Pertussis: Catarrhal phase, paroxysmal stage, and convalescent stage
-Catarrhal phase: earliest and lasts 1-2 weeks. Presents with malaise, rhinorrhea, and mild cough. Mild temperature may be present. May have some conjunctivitis and excessive lacrimation
-Paroxysmal phase: begins in the second week of the illness. Hallmark symptom is paroxysmal cough, in a series of severe, vigorous coughs that occur during a single inspiration. This is when the whooping sound is evident
-Convalescent phase-is characterized by a gradual reduction of frequency of the coughing. Usually lasts 1-2 weeks
-Complications of this illness include pneumonia, otitis media, subconjunctival hemorrhage, rib fractures, lumbar strain and urinary incontinence
-Most morbidity and mortality occur with infants and young children
-Bacterial culture and PCR are most useful clinical tools for confirmation of pertussis
-Macrolides are effective in eradicating pertussis, bactrim is an alternative treatment for those with macrolide allergy
-
Pneumonias-
-Pneumonia is defined as an infection of the lung parenchyma that is acute
-3 Categories of Pneumonia-
1. Community Acquired Pneumonia (CAP)- Acquired in the Community. Not acquired in hospital or health care setting
2. Hospital (Nosocomial) Acquired Pneumonia-aquired in the hospital
3. Healthcare Acquired Pneumonia (HCAP)-aquired in a nursing home, ambulatory surgical center or other health care facility (within 90 days of discharge from an acute or chronic care facility)
-Pathogenesis of pneumonia microaspiration of organisms in the lower respiratory tract
-Common clinical features is fever, pleuritic chest pain, dyspnea, sputum production. Rigors may also be present
-Chest auscultation reveals audible rales in the majority of the patient.
-Laboratory evaluation usually reveals leukocytosis with WBC between 15,000-30,000. Leukopenia implies poor prognosis
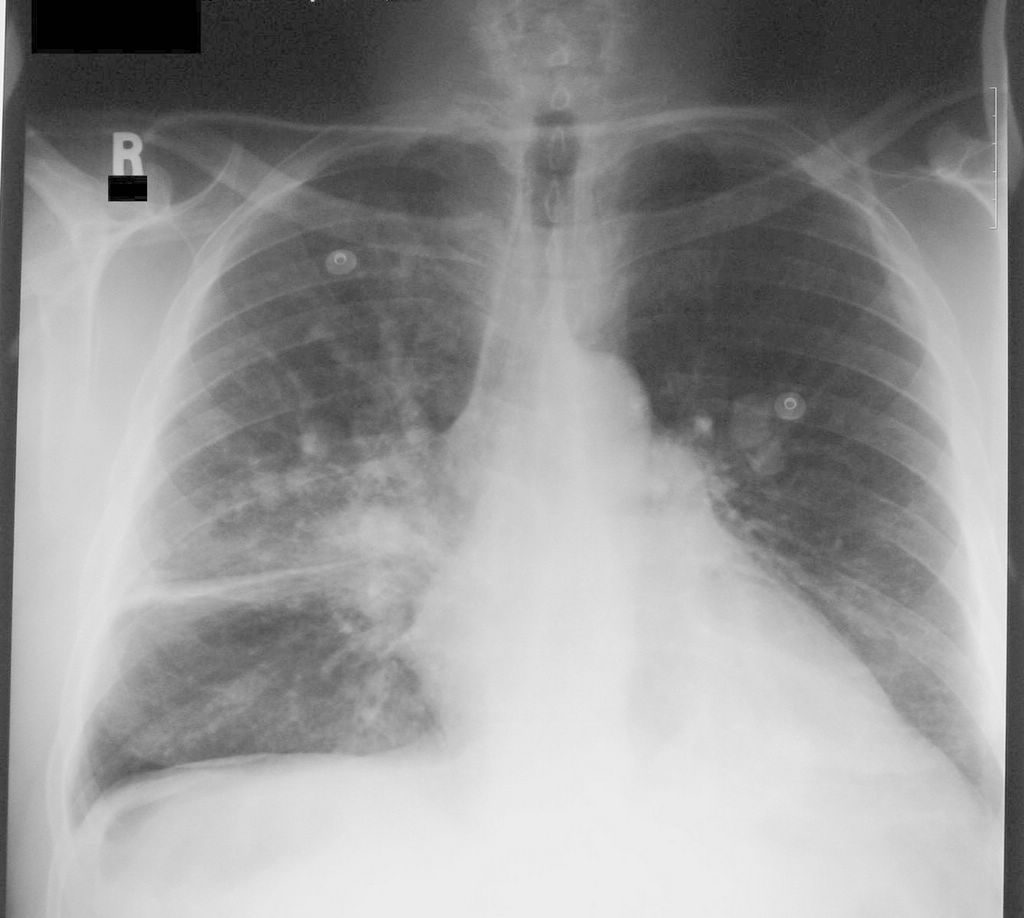
-The presence of an infiltrate on Chest X Ray is the gold standard for diagnosis of pneumonia.
-More than 100 organisms (bacteria, virus, and fungi, and parasites) can cause community acquired pneumonia
-Most common typical organisms causing community acquired pneumonia include: Strep Pneumonia, H. Influenza, S. Aureus, Group A Streptococci, Moraxella Catarrhalis, anaerobes, and gram negative bacteria.
-Atypical Organisms include: Mycoplasma pneumonia, Chlamydia pneumonia, Legionella, and C. Psittaci
-The most common organism causing community acquired pneumonia is Streptococcus Pneumonia
-Common viruses causes pneumonia include influenza virus, parainfluenza virus, respiratory syncytial virus, adenovirus, and coronavirus
-Fungi that cause community acquired pneumonia (usually in a immunocompromised patient) include Cryptococcus, Histoplasma Capsulatum, and Coccidioides
-Indications for hospitalization and severity of illness can be determined by the pneumonia severity index (PSI)
-Variables in PSI include: sex (male is worse), age, nursing home resident, comorbid illness (neoplastic disease, liver disease, heart failure, cerebrovascular disease, and renal disease), altered mental status, respiratory rate over 30, systolic blood pressure under 90 mmHg, temperature under 35 or over 40 degrees C, pulse over 125, arterial pH less than 7.35, BUN greater than 30, Sodium less than 130, blood sugar greater than 250, hematocrit less than 30, Pa02 less than 60, and pleural effusion
-Risk factors for antibiotic resistance include: age over 65, beta lactam, macrolide, or fluoroquinolone therapy within the past 3-6 months, alcoholism, medical comorbidity, immunosuppressive illness or therapy, or exposure to child in a daycare center
-For CAP outpatient treatment a macrolide or doxycycline is recommended.
-If there is a presence of comorbid problems, outpatient treatment with a fluoroquinolone, or beta-lactam should be used ouse a macrolide
-Inpatient non ICU patients with CAP a respiratory fluoroquinolone or a beta lactam should be used plus a macrolide
-ICU patients with CAP a beta-lactam plus azithromycin or a beta lactam plus a respiratory fluoroquinolone or a respiratory fluoroquinolone plus aztreonam
-If patients are at risk for pseudomonas an anti-pseudomonal beta-lactam plus cipro should be used with CAP. Another option is a beta lactam, plus aminoglycoside, plus azithromycin
-Hospital acquired pneumonia (HAP) occurs 48 hours or more after admission and did not appear to be incubating at time of admission
-Ventilator associated pneumonia (VAP)- develops more than 48-72 hours after intubation
-Common pathogens causing HAP, VAP, and HCAP include escherichia coli, klebsiella pneumonia, enterobacter, pseudomonas, acinetobacter, staphylococcus aureus, MRSA, and streptococcus
-Recommendations for HAP, VAP, and HCAP for no known risk factors for multiple drug resistance pneumonia: Ceftriaxone 2 grams daily, Unasyn 3.0 grams IV Q6, Levofloxacin or Avelox 400 mg IV or Ertapenem 1 gram IV daily
-If there is MDR risk factors above therapy plus one of the following for HAP, VAP, and HCAP cefepime, ceftazidime, meropenem, or zosyn
-If MRSA is suspected need to add Vancomycin, Linezolid, and Telavancin
-Three most common causes of fungal pulmonary pneumonia are: pneumocystis, aspergillus and cryptococcus pneumonia
-Pneumocystis is seen in transplant patients, HIV patients
-Pneumocystis is highly associated with cytomegalovirus infections
-Aspergillus can be present as a primary infection acquired from a nosocomial or environmental source or failure to already present in airways that are damaged by surgery or underlying source.
-Cryptococcus infections are appreciate when there is an asymptomatic pulmonary nodule or lymph node enlargement that occurs on a routine chest radiograph
-A large percentage of patients with cryptococcus infections are organ transplant recipients
-Candidia pneumonia is extremely rare
-Cytomegalovirus is the most common virus of concern with immunocompromised patients
-Slow or incomplete resolution of pneumonia despite treatment is common causing a high amount of pulmonary consults
-There are mechanical processes such as malignancy that can give the presence of an infiltrate
-Slow resolution is defined as radiographic abnormalities for 1 month after clinical improvement of the patient
-Bronchiolitis Obliterans Organizing Pneumonia (BOOP)- is a type of interstitial lung disease that affects distal bronchioles, respiratory bronchioles, alveolar ducts, and alveolar walls. The area of injury is the alveolar wall
-Often need steroids and other interventions with traditional antibiotics to get condition to improve
-
Respiratory Syncytial Virus (RSV) Infection-
-RSV infection causes acute respiratory illness in patients of all ages. In children, RSV usually results in a lower respiratory tract infection such as bronchiolitis
-In the Northern Hemisphere, RSV season is generally considered to be between November and April with a peak in January
-Risk factors for lower respiratory tract disease: infants less than 6 months of age, infants with bronchopulmonary dysplasia (BPD), premature infants greater than 35 weeks, infants with congenital heart disease, secondhand smoke, immunocompromised patients, asthma, residence of at an altitude over 2500 m, elderly patients.
-Transmission of RSV is by inoculation with nasopharyngeal or ocular mucous membranes after contact with virus containing hosts
-Incubation period is usually 6 days
-Almost all patients have been infected by the age of 3 but previous infection does not convey protection against recurrent infection
-RSV usually presents with cough, wheezing, purulent nasal drainage. Can have dyspnea, fever, and hypoxemia and signs of respiratory distress
-Clinical manifestations can include: apnea, comorbid bacterial infection, and can be associated with SIADH
-RSV is also likely to have more ear and sinus involvement than other viruses
-Diagnosis of RSV is generally suspected in patients with clinical symptoms during the correct season. Confirmed with nasal secretions and lab evaluation. Chest x ray may show bronchiolitis or pneumonia
-Can have concomitant bacterial infection, especially with pneumonia
-Treatment of RSV is largely supportive. Bronchodilators are indicated for children with wheezing or respiratory distress. Corticosteroids are recommended for children with RSV bronchiolitis or pneumonia
-Ribavirin aerosolized is not recommended for adults, children and infants with RSV causing lower respiratory tract infection
-Oxygen may need to be given for hypoxemia, and rarely some infants may require mechanical ventilation
-Synagis is a human monoclonal antibody against RSV F glycoprotein is for use in children younger than 24 months with BPD, preterm birth less than 35 weeks, or hemodynamically significant congenital heart disease
-
Tuberculosis-
-Tuberculosis (TB) is caused by the organism Mycobacterium Tuberculosis
-Signs and symptoms of TB include fever, productive cough, retrosternal pain, pleuritic pain, arthralgias, pharyngitis, and enlarged bronchial lymph nodes.
-90 percent of patients with normal immunity control further replication and enter a latent phase of TB
-The other 10 percent of patients develop TB pneumonia seeding near hilum, get hilar lymphadenopathy, may get cervical lymphadenopathy, meningitis, pericarditis, or get miliary dissemination
-Symptoms of reactivated TB include cough, hemoptysis, weight loss, fatigue, chest pain, dyspnea, and night sweats
-Findings on chest x ray with reactivation of disease include upper lobe cavitary lesions, hilar lymphadenopathy, and solitary nodules
-CT scans of the Chest is more sensitive for diagnosis the chest x-rays for TB
-Complications of TB include hemoptysis, pneumothorax, sepsis, bronchiectasis, extensive pulmonary destruction including gangrene, malignancy, and chronic pulmonary aspergilliosis
-Two tests available to for diagnosing latent TB infection: tuberculin skin test (TST) and interferon gamma release assay
-Indications for testing for latent TB include: close contacts of patients with active TB, casual contact of patients with highly contagious active TB, and healthcare workers and other occupations where there is a high risk of exposure with untreated contagious active TB (prisoners and homeless shelters)
-TST is used to show those that have been sensitized to mycobacterial antigens
-Induration for TST should be reassessed in 48-72 hours because is mediated by T Lymphocytes from a delayed hypersensitivity
-Interpretation of the test is as follows: greater than 5 mm induration is positive in HIV patients, close contact with an active case, abnormal chest x ray with findings of old TB, and immunosuppressed patients. Greater than 10 mm of induration is positive in patients with increase risk of reactivation, children less than 4 years, foreign born patients, residents and employees of high risk settings. Greater than 15 mm of induration is considered positive in healthy people with a truly low likelihood of true TB infection
-To diagnose active TB, clinical manifestations must be present. Generally a cough greater than 2-3 weeks, night sweats, weight loss, and lymphadenopathy. History of prior positive TST, and radiographic features and labs consistent with TB. It is recommended that the patient have at least three sputum specimens for acid fast bacillus (AFB)
-Patient should be respiratory isolation while being ruled out. Positive patients need to be reported to the local health department.
-Four drugs are used in the initial treatment o f active TB because of concern INH resistance. The 4 drugs are INH, rifampin, ethambutol, and pyrazinamide
-Duration of initial treatment lasts usually for 8 weeks. If culture and sensitive implicate sensitivity to one of the 4 agents, then ethambutol can usually be discontinued
-The continuation phases is administered for 4-7 months and usually consists of INH and Rifampin
-Hepatotoxicity needs to be monitored
-Need to reassess sputum culture after treatment to determine if there is treatment failure